6 mins read
What Is Type 2 Diabetes And Is It Preventable?

- What Is Prediabetes?
- What is Diabetes?
- Types of Diabetes
- Symptoms of Type 2 Diabetes
- What Causes Type 2 Diabetes?
- Physical Inactivity
- Genetics
In this blog, we look into prediabetes and the lifestyle changes you can make to reverse a prediabetes diagnosis.
What Is Prediabetes?
Diabetes can be a daunting and overwhelming diagnosis. There are different types of diabetes, each with their own unique symptoms and causes. In this article, we will explore the symptoms and causes of type 2 diabetes.
What is Diabetes?
Diabetes is a chronic disease that affects over 4 million people in the UK[1]. It is a condition that is caused by the body’s inability to produce or effectively use insulin, a hormone that regulates blood sugar levels. Diabetes can lead to serious health complications, including heart disease, kidney failure, and blindness. Management of the disease is critical to prevent these complications and maintain a healthy lifestyle.
Types of Diabetes
There are three main types of diabetes: type 1, type 2, and gestational diabetes. While all types involve issues with insulin production and regulation, the causes and management strategies can vary greatly.
In type 1 diabetes, the body’s immune system attacks and destroys the insulin-producing cells in the pancreas. This results in a complete lack of insulin, which is necessary to transport glucose from the bloodstream into the body’s cells for energy. Type 1 diabetes is typically diagnosed in childhood or adolescence and requires lifelong insulin therapy.
Type 2 diabetes, on the other hand, is caused by a combination of genetic and lifestyle factors that lead to insulin resistance. This means that the body’s cells become less responsive to insulin, making it difficult for glucose to enter the cells and be used for energy. Type 2 diabetes is often associated with obesity, physical inactivity, and poor dietary habits.
Gestational diabetes occurs during pregnancy and typically resolves after delivery. It is caused by hormonal changes that affect insulin sensitivity and can increase the risk of complications for both the mother and baby. Women who develop gestational diabetes are at higher risk of developing type 2 diabetes later in life.
Symptoms of Type 2 Diabetes
Common symptoms include frequent urination, increased thirst, and constant hunger. People with type 2 diabetes may also experience unexplained weight loss, fatigue, blurred vision, slow-healing wounds, and recurring infections. Some individuals might have patches of darkened skin in certain areas, a condition known as acanthosis nigricans. If left untreated, type 2 diabetes can lead to serious complications affecting the heart, blood vessels, kidneys, and eyes. Early diagnosis and proper management through lifestyle changes and medications are essential to prevent complications and maintain overall health.
What Causes Type 2 Diabetes?
Type 2 diabetes, which accounts for about 90% of all diabetes cases, is largely preventable. There are a variety of risk factors that can contribute to the development of type 2 diabetes, including:
Obesity
Obesity is one of the biggest risk factors for type 2 diabetes. When you are overweight, your body becomes less sensitive to insulin, which can lead to high blood sugar levels. In addition, excess body fat can cause inflammation, which can also contribute to insulin resistance. Losing weight through a healthy diet and regular exercise can significantly reduce your risk of developing diabetes.
Physical Inactivity
Physical inactivity is another major risk factor for diabetes. When you don’t exercise regularly, your muscles become less sensitive to insulin, which can lead to high blood sugar levels. Exercise helps your body use insulin more effectively, which can lower your risk of developing diabetes. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Genetics
While lifestyle factors play a big role in the development of type 2 diabetes, genetics also play a role. If you have a family history of diabetes, you may be more likely to develop the condition yourself. However, this does not mean that you are destined to develop diabetes. By making healthy lifestyle choices, you can reduce your risk of developing the condition, even if you have a family history of diabetes.
Other risk factors for diabetes include age, race, and certain medical conditions such as high blood pressure, high cholesterol and PCOS. By identifying these risk factors and making appropriate lifestyle changes, individuals can reduce their risk of developing diabetes and live a healthier, happier life.
How Insulin Works in the Body
Insulin is a hormone that is produced by the pancreas. Its primary function is to help regulate blood sugar levels in the body. When we eat, our bodies break down the food into glucose, which is then transported through the bloodstream to our cells. Insulin helps to move the glucose from the bloodstream into the cells, where it can be used for energy.
The Role of Glucose in Diabetes
Glucose is the main source of energy for the body’s cells. It is a type of sugar that is produced when we eat carbohydrates. In individuals with diabetes, the body is unable to effectively regulate glucose levels, leading to elevated levels in the bloodstream. Over time, high blood sugar levels can cause damage to various organs and systems in the body.
Potential Complications of Diabetes
One of the most common complications of diabetes is cardiovascular disease. High blood sugar levels can damage the blood vessels and nerves that control your heart and blood vessels, increasing your risk of heart attack, stroke, and other cardiovascular problems.
In addition to cardiovascular disease, diabetes can also cause nerve damage, a condition known as diabetic neuropathy. This can lead to numbness, tingling, and pain in the hands and feet, as well as other parts of the body. Over time, diabetic neuropathy can also cause muscle weakness and difficulty walking.
Another potential complication of diabetes is vision loss, which can occur as a result of damage to the blood vessels in the eyes. This can lead to a range of vision problems, including blurred vision, double vision, and even blindness in severe cases.
It is important to manage diabetes closely in order to reduce the risk of these complications and maintain overall health and wellness. This includes monitoring your blood sugar levels regularly, following a healthy diet and exercise plan, and taking any medications as prescribed by your doctor.
Other steps you can take to manage your diabetes and reduce the risk of complications include quitting smoking, maintaining a healthy weight, and getting regular check-ups with your healthcare provider. By taking these steps, you can help to prevent or delay the onset of complications and maintain a good quality of life with diabetes.
Is Type 2 Diabetes Preventable
While type 2 diabetes is a complex disease with a variety of contributing factors, there are steps that individuals can take to reduce their risk of developing the condition. You can increase your chances of preventing type 2 diabetes by:
Exercising – aim for at least 30 minutes of moderate exercise a day. This could be anything from a brisk walk to cycling or swimming.
Eat a Balanced Diet – Maintaining a balanced diet that is rich in fruits, vegetables, whole grains, and lean proteins while limiting the consumption of sugary and processed foods can help manage weight and blood sugar levels.
Avoid Alcohol & Smoking – Excessive drinking and smoking can increase your risk of developing type 2 diabetes[2].
Get Good Sleep – good quality sleep supports overall health, and lack of sleep has been linked to obesity, which is a leading factor in developing type 2 diabetes.
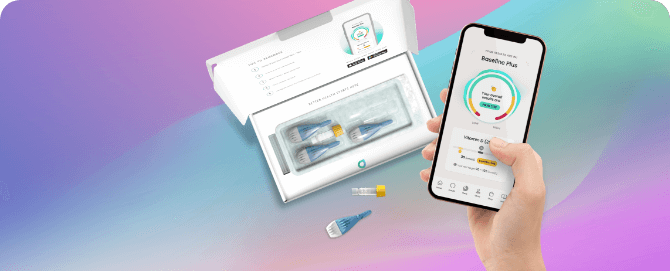
Regular testing – Keeping track of your blood sugar levels will help you prevent or monitor diabetes. Regular blood testing is an easy and effective way of staying in control of your health.
Type 2 diabetes can be reversed if you can fortify new habits and make the lifestyle changes listed above.
- Health scores calculated
Close
Article references
-
Rynders, C, A et al. (2014). Effects of Exercise Intensity on Postprandial Improvement in Glucose Disposal and Insulin Sensitivity in Prediabetic Adults. The Journal of Clinical Endocrinology and Metabolism: 99(1), pp 220-228.
-
Tuso, P. (2014). Prediabetes and Lifestyle Modification: Time to Prevent a Preventable Disease. Perm J: 18(3), pp 88-93.
This information has been medically reviewed by Dr Thom Phillips
Thom works in NHS general practice and has a decade of experience working in both male and female elite sport. He has a background in exercise physiology and has published research into fatigue biomarkers.

Dr Thom Phillips
Head of Clinical Services
Related articles
Like this article? Here are some more based on similar topics.