7 mins read
UK Vitamin D Statistics 2024: 57% of Brits Have Low Vit D Levels

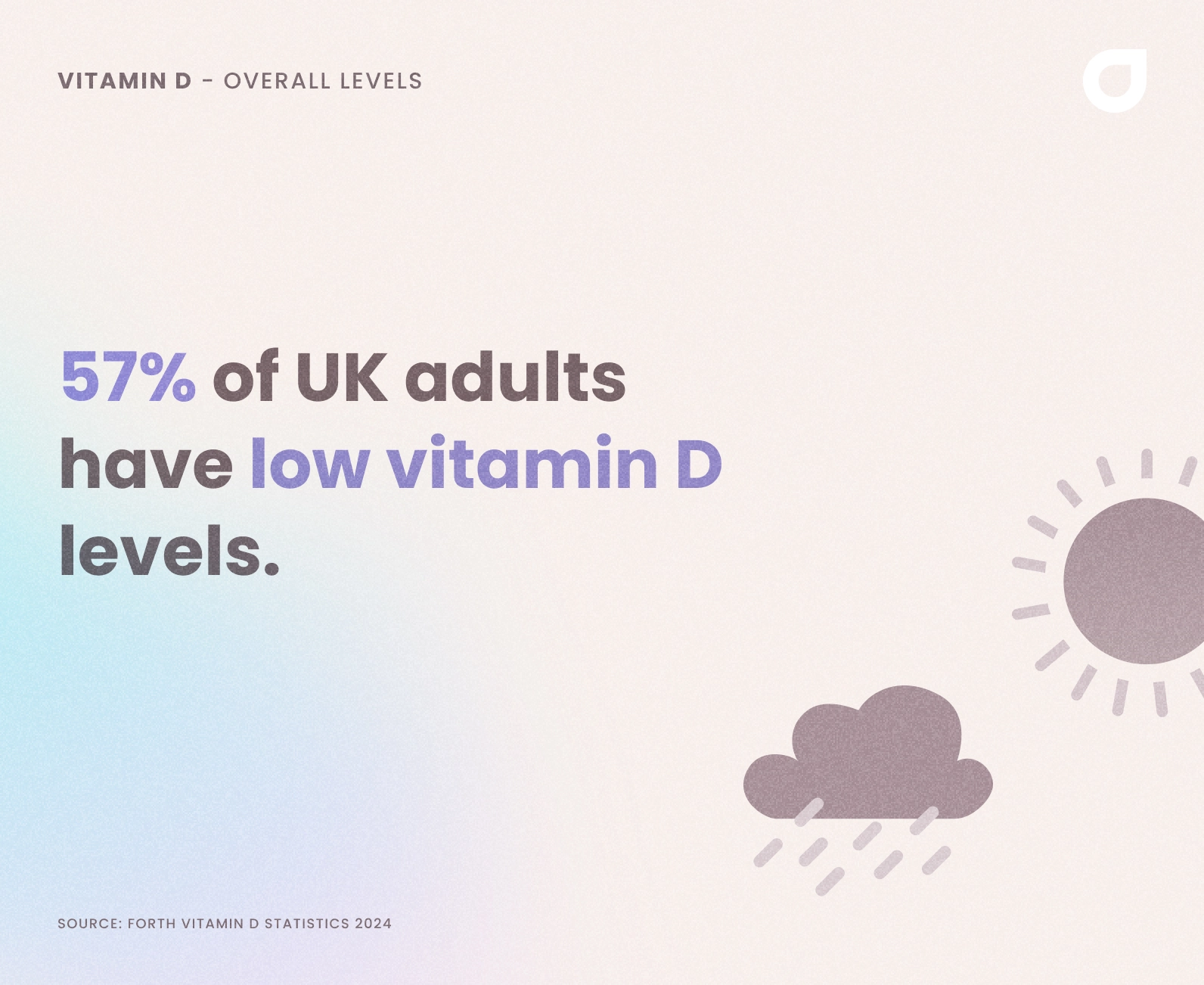
Vitamin D is one of the most important nutrients for our health. But, it’s also one that most of us don’t get enough of. We looked at vit D levels in Brits in 2018, 2020 and 2023, and again in April 2024. We’ve found the trend has continued, with 57% of UK adults having below-optimal levels of vitamin D.
Short on time? Here’s a summary of our 2024 vitamin D statistics
- 57% of UK adults have below-optimal levels of vitamin D
- The average vitamin D level is 78.7 nmol/L
- There was a 3.2nmol/L difference in vitamin D levels between men and women, with women having a slightly lower level at 77.2 nmol/L, compared to 80.4 nmol/L for men
- Adults aged 18-29 had the lowest average levels (71.9 nmol/L) and the highest percentage of low levels (62%)
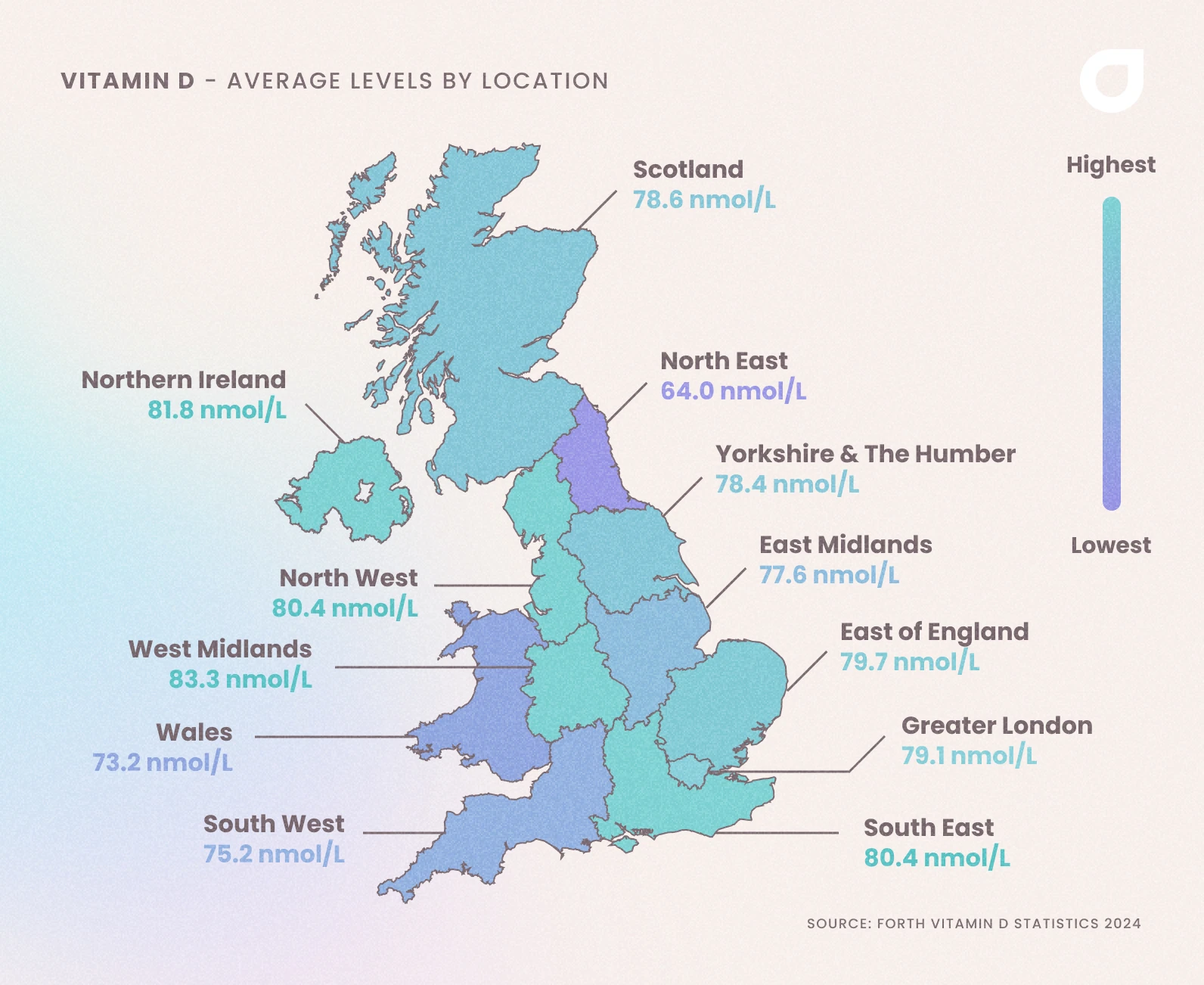
- People in the West Midlands had the highest average vitamin D levels at 83.3 nmol/L
- People in the North East had the lowest average levels (64 nmol/L)
- Bradford was the best city in the UK, with an average level of 101.8 nmol/L
Why is Vitamin D Important?
Before we dive into the statistics, it’s helpful to understand why vitamin D is important, from our bones and immune system to our mental health and muscle function.
-
Immune System
Vitamin D is involved in the functioning of the immune system. It helps modulate immune responses, and its deficiency has been linked to an increased susceptibility to infections and autoimmune diseases.
-
Cell Growth and Regulation
Vitamin D helps to regulate cell growth. Adequate levels of vitamin D are associated with a decreased risk of certain cancers[1] and may contribute to overall cellular health.
-
Mood and Mental Health
Some research suggests that vitamin D may have a role in mood regulation and mental health[2]. Deficiency has been linked to conditions such as seasonal affective disorder (SAD) and depression.
-
Heart Health
There is evidence suggesting that vitamin D may play a role in cardiovascular health[3]. It is associated with improved blood vessel function and may have a protective effect against heart disease.
-
Muscle Function
Vitamin D is important for muscle function and may help prevent muscle weakness and pain.
-
Bone Health
Vitamin D is essential for the absorption of calcium and phosphorus in the intestines. Without enough vitamin D, the body cannot properly absorb calcium, leading to weakened bones and an increased risk of fractures and osteoporosis.
Why Don’t We Get Enough?
During the summer, we get most of our vitamin D from the sun.
Ultraviolet B rays from the sun kick off a process that converts certain types of cholesterol into previtamin D3, an inactive form of vitamin D.
Warmth, such as the heat from the sun, then converts this into active D3, which gets transported to our liver and kidneys before being sent around our body as calcitriol.
We struggle to get enough vitamin D from the sun during the autumn and winter, as the sun is much less powerful and the days are a lot shorter. This leads to a deficiency, which can cause illness, fatigue and cause conditions like SAD.
Only a handful of foods contain vitamin D (oily fish, red meat, liver, egg yolk and fortified cereals), so it can be hard to get enough from our diet alone. Supplementation can help, such as a daily vitamin or spray.
How Much Do We Need?
There are different recommended levels of vitamin D depending on where you look or who you ask.
Most experts agree a minimum level somewhere between 70 and 80 nmol/L.
For this study, we classed levels below 75 nmol/L as “low”.
Adults and children over 4 years old need 10 micrograms (400 IU) of vitamin D per day to maintain healthy levels. From birth to 4 years old, NICE recommends using a daily vitamin d supplement drop[4].
How Many Of Us Are Low On Vit D?
We looked at data from 1,400 Forth customers between January 1st 2024 and 31st March 2024 to see how many people are low on vitamin D.
We found that 57% of people had a vitamin D level below the optimal range (75-100 nmol/L). The average level was 78.7 nmol/L.
Men had higher average levels than women, at 80.4 nmol/L. Women’s average vitamin D levels were 77.2 nmol/L, just above the minimum level of 75 nmol/L.

"This backs up the consensus that most people in the UK are Vitamin D deficient. This particularly affects non-Caucasian people as the increased melatonin in the skin. the current guidelines suggest that all people need a minimum of 400iu a day, but as we’re not all the same, checking your levels first is a great place to start to understand your individual vitamin D needs."
Dr Thom Phillips
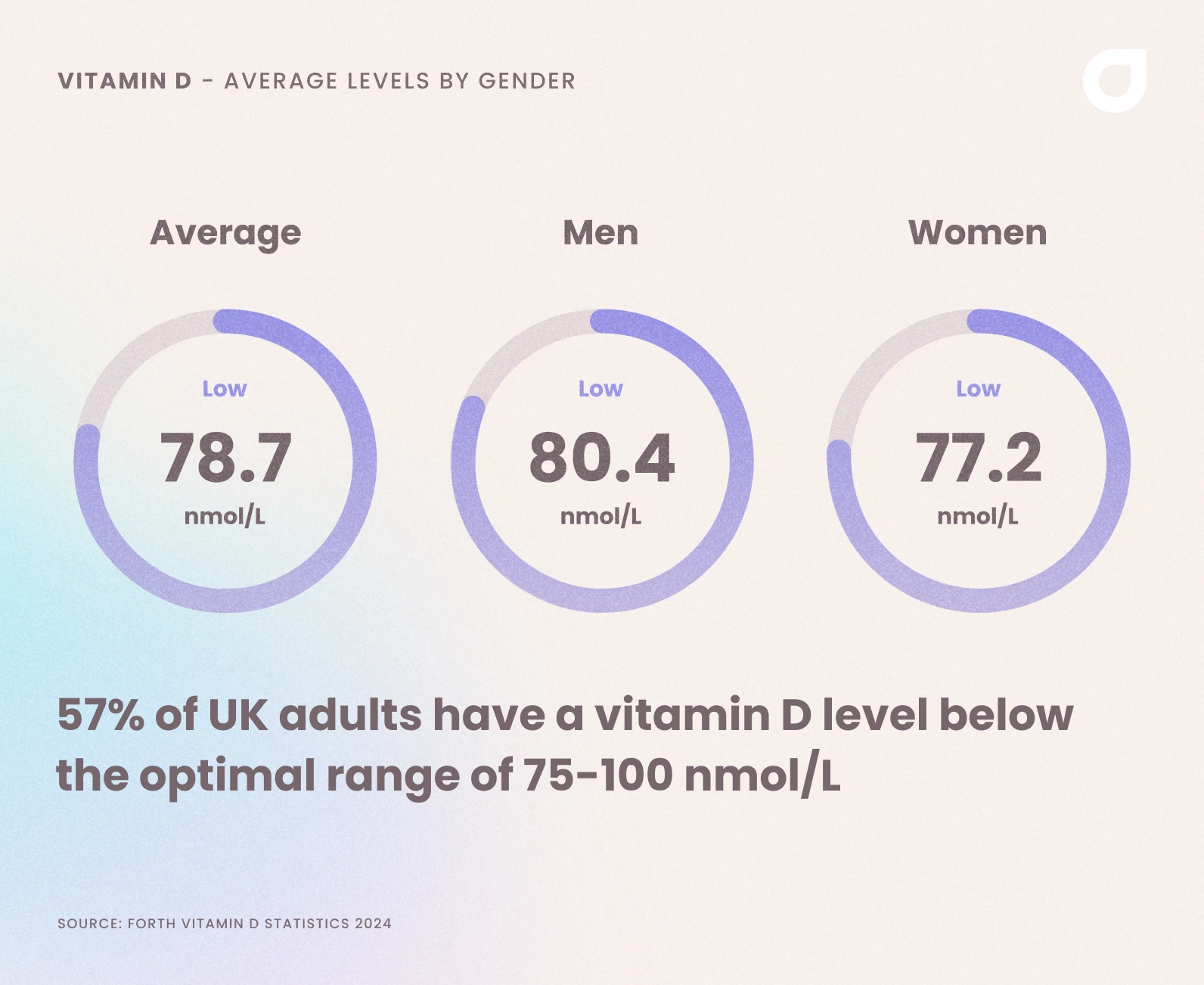
57% of men and women had vitamin D levels below the optimal range
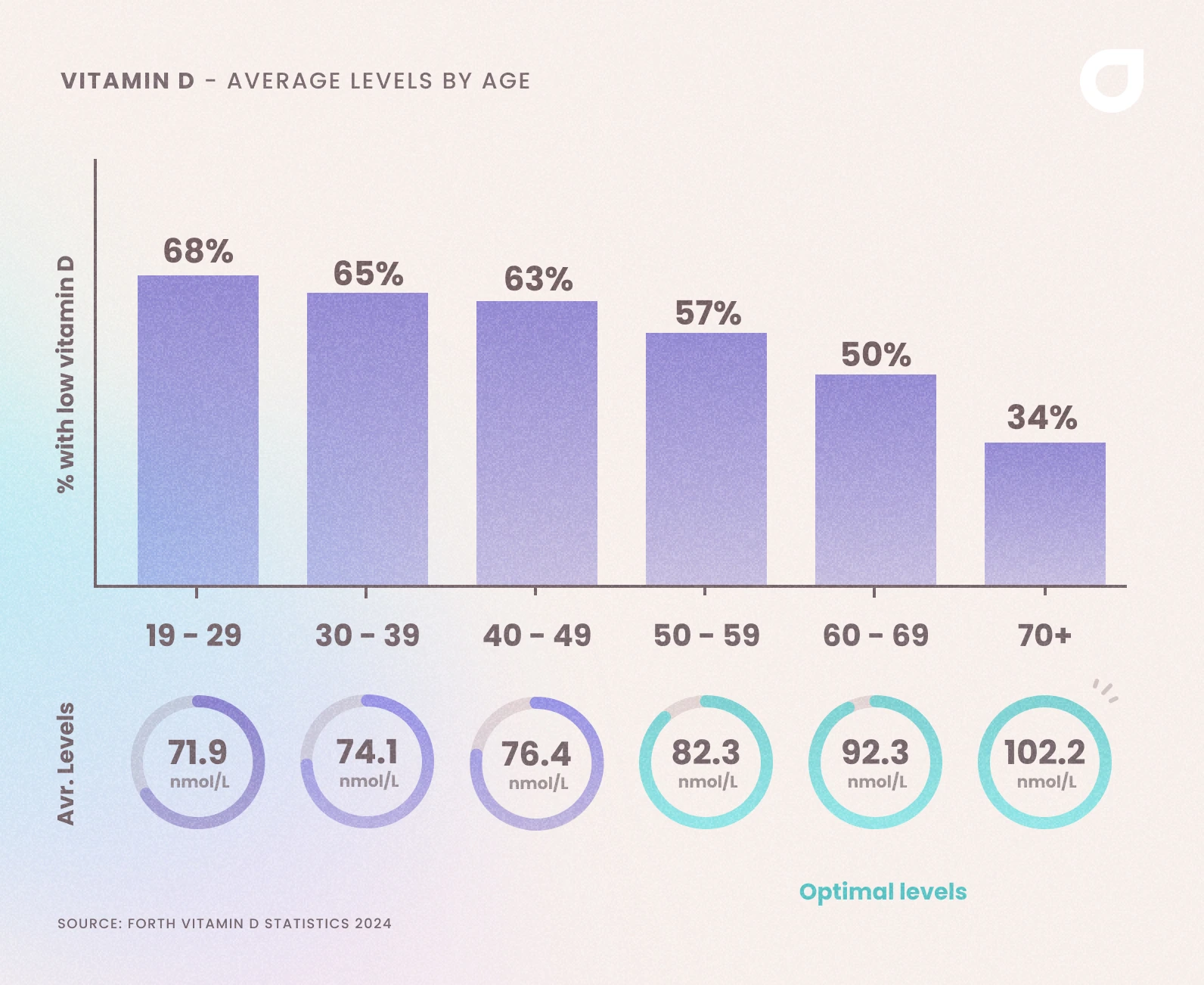
We also broke the data down to look at age groups. We found that those aged 18-29 had the lowest average levels and the highest percentage of low levels.
The data shows that the older we get, the better our vitamin D levels get, with the over 60s having an average level of 86.5 nmol/L. – over 20 nmol/L higher than the 18-29 year olds.
| Age Bracket | Percentage Low | Average Level (nmol/L) |
| 18-29 | 62% | 73.3 |
| 30-39 | 62% | 74 |
| 40-49 | 58% | 75.4 |
| 50-59 | 52% | 82.6 |
| 60+ | 41% | 96.5 |
It seems the older we get, the better our vitamin D levels are. Perhaps this is because we’re able to spend more time enjoying the outdoors after we retire or are more health conscious as we get older.

"Looks like our customers are enjoying their retirement! There are also a proportion of older people who will be prescribed vitamin D supplements by their GP so it’s not too surprising that the older demographic have better levels. Also this may reflect that all of us are terrible at understanding long term risks, and are less inclined to make positive health choices when we’re younger."
Dr Thom Phillips
Is Location A Factor?
We also wanted to know if where we live plays a role in our vitamin D levels. Does living in the countryside mean you get more vitamin D than those living in busy urban areas?
First of all, let’s look at the average vitamin D level by region:
| Region | Percentage of People with Low Vitamin D | Average Level (nmol/L) |
| West Midlands | 58% | 83.3 |
| Northern Ireland | 57% | 81.8 |
| South East | 60% | 80.4 |
| North West | 62% | 80.4 |
| East of England | 62% | 79.7 |
| Greater London | 58% | 79.1 |
| Scotland | 59% | 78.6 |
| Yorkshire and the Humber | 56% | 78.4 |
| East Midlands | 69% | 77.6 |
| South West | 62% | 75.2 |
| Wales | 60% | 73.2 |
| North East | 73% | 64 |
The average level for the whole of England was 79 nmol/L.
People in Northern Ireland had the highest average vitamin D levels at 83.3 nmol/L, followed by those in Northern Ireland (81.8 nmol/L) and the East of England (79.7 nmol/L).
The North East (64 nmol/L), Wales (73.2 nmol/L) and the South West (75.2 nmol/L) had the lowest average levels.
This shows that where you live may have an effect on your vitamin D levels, but as all regions are still below the optimal range, it’s safe to say that no matter where you live in the UK, you may still struggle to get enough.
Which Cities Have The Best Vitamin D Levels?
We looked at which UK cities have the highest average vitamin D levels and found that Bradford was the best – with an average level of 98 nmol/L.
8 cities had average levels within the optimal range – up for just 4 in 2023.
Below are the top 20 cities by average vit D levels.
| City | Average Vit D Level (nmol/L) |
| Bradford | 98 |
| Oxford | 94 |
| Kent | 94 |
| Birmingham | 93.7 |
| Norwich | 89.8 |
| Southampton | 85 |
| Manchester | 84.2 |
| Reading | 80.4 |
| Surrey | 79 |
| London | 78.6 |
| Sheffield | 77.4 |
| Edinburgh | 77.3 |
| Glasgow | 77 |
| Liverpool | 69.2 |
| Newcastle Upon Tyne | 68.4 |
| Cardiff | 62.9 |
| Nottingham | 61.5 |
| Bristol | 56 |
| Aberdeen | 49.1 |
| Stockport | 49 |
How to Increase Your Vit D Levels
The best way to increase and maintain your vitamin D levels, especially during the winter, is to get as much sunlight as you can, take a daily supplement and ensure you’re eating foods that contain vit D.
Make sure to read the labels of any supplements you’re thinking of buying, as many are underdosed – meaning they don’t offer as much vitamin D as you need.
There is some research that suggests endurance exercise, such as running and cycling, can increase serum vitamin D levels, too[5].
How Can I Check My Vitamin D Level?
A blood test is the best way to check your vitamin D levels. Our vitamin D blood test is an at-home, finger prick test. That means there are no needles – just collect a small sample of blood from your fingertip using the lancets included in the kit, and post it back to our NHS labs for analysis.
We also offer more comprehensive tests, like our Baseline Health Check, which not only checks your vitamin D levels, but a whole range of other biomarkers that can affect your energy, immune system, bone health and more.
Two-thirds of customers increased their vitamin D level after using testing at home with our blood tests.
Can Tanning Beds Help With Low Vit D?
Although it might seem like a good idea during the winter, tanning beds are not an effective or safe way to boost your vitamin D levels. We use Ultraviolet B (UVB) to produce vitamin D from the sun, but tanning beds use Ultraviolet A (UVA), which penetrates deep into the skin and can cause skin cancer.
What Supplements Are Best?
At Forth we always try to promote a food (and in this case, safe sun!) first approach. However, we also need to acknowledge that sometimes supplements may be a quicker and more convenient way to ensure you’re hitting your nutrient targets.
In the UK, vitamin and mineral supplements are classed as food, not medicines, and as such do not always meet the high safety standards expected of a medicine.
Always use a reputable retailer and check the labels carefully for allergens, additives and flavour enhancers. I usually recommend people use Informed Sport (https://www.wetestyoutrust.com/) labelled products. These are independently batch-tested and accredited, so you know you’re getting a quality product.
Do Pregnant Women Need More Vitamin D?
As well as being important for the mother, vitamin D helps with foetal development, making it an important nutrient for both mother and baby. The NHS recommends pregnant women take a daily supplement between September and March, and keep to 10 micrograms a day.
- Health scores calculated
Close
This information has been medically reviewed by Dr Thom Phillips
Thom works in NHS general practice and has a decade of experience working in both male and female elite sport. He has a background in exercise physiology and has published research into fatigue biomarkers.

Dr Thom Phillips
Head of Clinical Services
Related articles
Like this article? Here are some more based on similar topics.