7 mins read
What is Osteoporosis: Causes, Symptoms and Treatment

What is osteoporosis?
Osteoporosis is a common bone disease, characterised by the loss of bone mass and deterioration of bone tissue. It is often called the “silent disease” because it progresses silently and without symptoms until a fracture or break occurs. Osteoporosis mainly affects older people, especially women after menopause, but it can also occur in younger individuals.
According to the NHS, around 3 million people in the UK have osteoporosis[1], with the condition being four times more common in women than men[2].
What is osteopenia?
Osteopenia is a precursor to osteoporosis and refers to low bone mass that is not severe enough to be classified as osteoporosis. Identifying osteopenia early provides an opportunity to prevent the progression to osteoporosis through lifestyle modifications and medicine.
Forth’s founder, Sarah, shares her story on diagnosing osteopenia, HRT and bone health.
What causes osteoporosis and osteopenia?
Bone density naturally decreases with age, but women can be particularly susceptible to a rapid reduction in bone density (osteopenia) in the first few years after menopause, due to hormonal changes.
Oestrogen plays a major role in protecting your bone density. But, levels decline during menopause, causing reduced bone density and increased risk of fractures.
Your diet can also impact your likelihood of developing osteoporosis. Calcium is an essential mineral for maintaining strong bones, and vitamin D helps the body absorb calcium effectively. Without sufficient amounts of these nutrients, our bones become more susceptible to fractures and deterioration.
Regular weight-bearing exercises, such as walking, jogging, or weightlifting, help stimulate bone growth and maintain bone density. When we don’t engage in these activities, our bones may become weaker and more prone to fractures. Research has shown that resistance training (weightlifting) has a direct impact on not only our muscles, but bones too[3].
“Regular, weight bearing exercise, as well as strength based exercise is probably the most important thing you can do to look after your bone health. Minimise the time you sit on a daily basis as even standing can be beneficial. The Royal Society of Osteoporosis has some excellent resources regarding exercise if you’ve already been diagnosed with Osteoporosis.“
Dr Thom Phillips
Unhealthy habits like smoking and excessive alcohol consumption can also contribute to the development of osteoporosis. Smoking has been linked to lower bone density[4] and an increased risk of fractures. Similarly, excessive alcohol consumption can interfere with the body’s ability to absorb calcium, leading to weakened bones.
Other causes of osteoporosis can also include: taking medications that reduce bone density, family history of osteoporosis (genetics), having bulimia or anorexia eating disorders, a low BMI and thyroid disorders.
Symptoms of osteoporosis
Osteoporosis is often asymptomatic (it has no symptoms), but there are some signs that may indicate its presence.
Some people with osteoporosis may develop a stooped posture. This is known as kyphosis, and is more common in older people. The weakening of the bones in the spine can cause it to curve forward, resulting in a rounded upper back and a hunched appearance.
Osteoporosis makes bones more fragile and susceptible to fractures. Even minor falls or accidents that would not typically cause a fracture can result in broken bones. Fractures commonly occur in the hip, wrist, and spine, and can be extremely painful and debilitating.
“Fragility fractures (broken bones with underlying bone thinning) are a massive health issue. As well as being hugely inconvenient, often we can use a fragility fracture as a marker of overall health and, perhaps surprisingly, having a fragility fracture doubles the risk of death in the following year for older women and triples the risk in older men[5].”
Dr Thom Phillips
Diagnosing osteoporosis
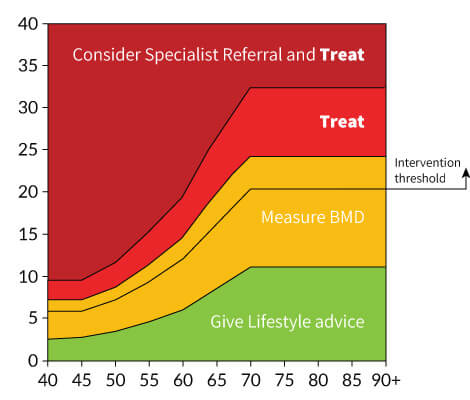
To assess your risk of having osteoporosis or osteopenia your doctor may initially use a risk stratification tool known as a FRAX score which was developed by the University of Sheffield.
The FRAX score assesses the 10-year probability of a person experiencing a major osteoporotic fracture or hip fracture. It considers factors such as age, gender, body mass index, previous fractures, parental hip fractures, smoking, glucocorticoid use, rheumatoid arthritis, and alcohol intake.
Calculated through a web-based tool, a higher FRAX score indicates an increased risk of fracture, aiding clinicians in determining the need for osteoporosis treatment or diagnostic investigations. (The National Osteoporosis Guideline Group (NOGG-UK) then translate your FRAX score into an advised next steps.).
The most common diagnostic investigation for the presence of osteoporosis is usually made through a bone density scan, also known as a DEXA scan. This non-invasive test measures bone mineral density and helps determine the risk of fractures. The results are given as a T-score, with values below -2.5 indicating osteoporosis.
During a DEXA scan, a machine scans your hip and spine, the most common sites for osteoporotic fractures. It only takes a few minutes to complete and then results are then analysed by a radiologist or a specialist in bone density interpretation.
A DEXA scan is not the only method used to diagnose osteoporosis. In some cases, additional tests may be required to confirm the diagnosis or to assess the underlying causes of bone loss. These tests may include blood tests to measure calcium and vitamin D levels, as well as other bone turnover markers.
Once a diagnosis of osteoporosis is confirmed, further evaluation may be necessary to determine the severity of the condition and to identify any underlying factors that may be contributing to bone loss. This may involve additional imaging tests, such as X-rays or magnetic resonance imaging (MRI), to assess the structural integrity of the bones and identify any existing fractures.
Your doctor will also talk to you about any previous fractures, family history of osteoporosis, and any medications or medical conditions that may increase the risk of bone loss. They may also assess your lifestyle factors, such as diet, exercise habits, and smoking or alcohol consumption, as these can significantly impact bone health.
Treating osteoporosis
Treating osteoporosis involves a combination of lifestyle modifications and medications. Calcium and vitamin D supplements are commonly recommended to ensure adequate bone nutrition. In some cases, hormone therapy may be used in postmenopausal women to counteract the decline in oestrogen levels.
There are also a variety of medications available to prevent further bone loss and increase bone strength. The choice of medication depends on individual factors, such as the severity of osteoporosis and any underlying medical conditions. Your doctor will be able to advise on what’s best for you.
How can you prevent osteoporosis?
Preventing osteoporosis begins with a proactive approach to bone health. A balanced diet rich in calcium and vitamin D is essential for bone strength. Good food sources of calcium include dairy products, leafy greens, and fortified foods. Vitamin D can be obtained from sunlight exposure and certain foods like fatty fish and eggs.
Regular physical activity, particularly weight-bearing exercises, helps improve bone health and reduces the risk of fractures. Avoiding tobacco smoking and excessive alcohol consumption can also help maintain bone density.
Why do our bones get weaker?
Our bones are not just static structures that provide support and protection to our bodies; they are living tissues that undergo a constant process of remodelling. This remodelling involves the removal of old bone tissue by cells called osteoclasts and the formation of new bone tissue by cells called osteoblasts.
However, sometimes this delicate balance between bone resorption and bone formation can be disrupted, leading to conditions like osteopenia. Osteopenia is often asymptomatic, meaning that it does not cause any noticeable symptoms.
“Bone remodelling is regulated by various cytokines (a type of immune protein), growth factors, and signalling pathways. The most important pathways in the bone remodelling model is the nuclear factor-kappa B (RANKL) pathway, crucial for osteoclast differentiation and activation. Osteoprotegerin (OPG), acts as a brake on excessive bone resorption. Imbalances in the RANKL/OPG ratio can tip the scale towards increased bone resorption.
Up until your 30’s, the balance lies slightly in favour of new bone being laid down, but from around the age of 30 in men and 35 in women this balance begins to shift the other way. If measures such as weight bearing exercise, good diet and avoiding smoking and alcohol are not adopted then this balance can slide to the point that your bone density starts to reduce. Eventually, if this process is not stopped your bones begin to thin.”
Dr Thom Phillips
- Health scores calculated
Close
Article references
-
Brown JP, Adachi JD, Schemitsch E, Tarride JE, Brown V, Bell A, Reiner M, Oliveira T, Motsepe-Ditshego P, Burke N, Slatkovska L. Mortality in older adults following a fragility fracture: real-world retrospective matched-cohort study in Ontario. BMC Musculoskelet Disord. 2021 Jan 23;22(1):105. doi: 10.1186/s12891-021-03960-z. PMID: 33485305; PMCID: PMC7824940.
This information has been medically reviewed by Dr Thom Phillips
Thom works in NHS general practice and has a decade of experience working in both male and female elite sport. He has a background in exercise physiology and has published research into fatigue biomarkers.

Dr Thom Phillips
Head of Clinical Services