Build your own
Build your own test that's specific to your health needs, choosing from our wide range of Biomarkers.
Choose from 30+ markers
14 mins read
Perimenopause & Menopause: What are they and what are the symptoms?
- What are the stages of menopause?
- WHAT IS MENOPAUSE?
- What is Post-menopause?
- How to know if you’re going through perimenopause or menopause
- How does each stage impact fertility?
Menopause is a natural part of life and is a gradual biological process that all women go through. However, in today’s modern world where we have a longer life expectancy, women are spending more of their life in post-menopause.
Therefore, it is important that women are informed about the menopause, the potential long-term health issues caused by changes in hormone levels, and the options available to help manage menopause symptoms and maintain quality of life post-menopause.
What are the stages of menopause?
There are three stages of menopause that women go through; perimenopause, menopause and post-menopause. Each stage comes with its own symptoms and challenges for women. You can check your hormone levels with our Menopause Test Kit.
WHAT IS PERIMENOPAUSE?
Perimenopause is the phase that leads to menopause. Women tend to start perimenopause in their early 40s and it can last anywhere between 5 and 10 years. The symptoms of perimenopause are often wrongly associated with menopause.
Unsure if you’re perimenopausal? Use our interactive perimenopause symptom checker to gain more insight.
WHAT IS MENOPAUSE?
Menopause is the point in time when ovulation stops, usually defined when a woman has not had a period for 12 months or more. On average, women reach menopause between 45 and 55 years of age. Perimenopause, the phase leading to menopause, can start as early as 40. Perimenopausal symptoms can last for up to 4 years after you’ve entered the menopause.
Early menopause is when periods stop at the age of 40, but before the age of 45. Approximately 1 in 20 women experience menopause before the age of 45. Premature ovarian insufficiency (POI) is where menopause occurs before age of 40 years.
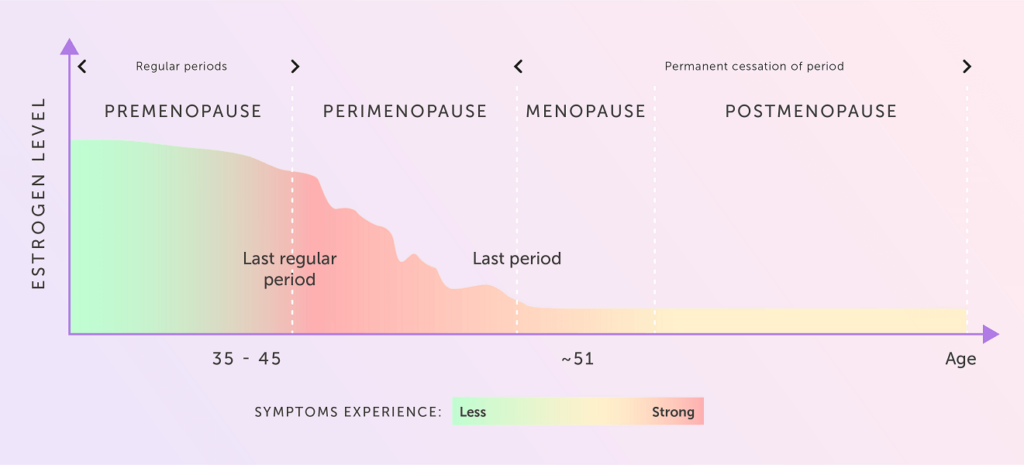
What is Post-menopause?
Post-menopause is the term used to describe the time period after the menopause when menstruation has ceased.
How to know if you’re going through perimenopause or menopause
Generally, perimenopause is diagnosed based on symptoms and once all other possibilities have been excluded. Until now, blood tests have only measured hormones at a single point in time, usually day 3, and therefore do not map out the fluctuations in hormones and the complex interplay between the control and ovarian response hormones.
We’ve developed the only blood test in the world that can confirm if the symptoms you are experiencing are due to perimenopause.
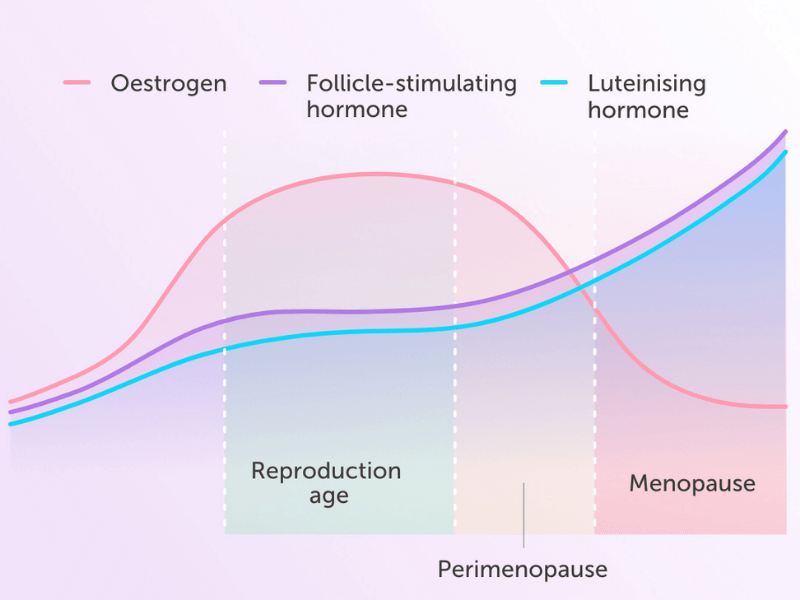
Our unique perimenopause home blood test, MyFORM™, measures follicle-stimulating hormone (FSH), luteinising hormone (LH), oestrogen and progesterone. By combining blood analysis with artificial intelligence and clinical expertise, we are able to map out your hormones across an entire menstrual cycle. This enables us to provide you with your own, personalised hormone curves across your menstrual cycle. From this, you will be able to see if your ovaries are less responsive to the two control hormones.
How does each stage impact fertility?
As you transition through to the menopause, your periods will become irregular and ovulation less certain, making it more difficult to become pregnant. This is due to your ovaries becoming less responsive to your two control hormones – follicle-stimulating hormone (FSH) and luteinising hormone (LH) – that trigger your ovaries to produce oestrogen and progesterone. The results of declining levels of oestrogen and progesterone are increased levels of FSH and LH.
However, it is still possible to become pregnant during perimenopause, as ovulation can occur even if your periods are irregular or without having a period. So, if you are not planning on having children you should continue to use a contraceptive.
“With reduced ovarian responsiveness comes sporadic ovulation and hence reduced fertility”,
– Dr Nicky Keay.
Your Hormones During Perimenopause and Menopause
The main hormones that change as you transition to menopause are the two ovarian hormones which are oestrogen and progesterone; and the two control hormones which are follicle-stimulating hormone (FSH) and luteinising hormone (LH). It is the declining levels of oestrogen that cause many of the symptoms associated with perimenopause, with raises in FSH disrupting temperature regulation.
Your FSH levels rise and fall throughout your menstrual cycle, but will start to increase as you transition through the perimenopause phase and to menopause.
Your oestrogen levels will continue to decline during menopause, until levelling off a low level. In contrast, FSH and LH levels will continue to rise.
Perimenopause & Menopause Symptoms
Although it’s common to refer to menopause symptoms, it’s actually the transition phase called perimenopause that causes the majority of symptoms.
Perimenopausal symptoms can start months or years before your periods stop and last for up to 4 years after. There are over 34 different symptoms women experience, but you may not experience them all:
As the responsiveness of the ovaries starts to decrease, the hormones that are produced declines. Furthermore, oestrogen and progesterone can become unbalanced. For example, intermittent anovulatory cycles (missed periods) results in lower levels of progesterone over a cycle. So in the early stages of the transition to the menopause, periods may become irregular and change in nature. You may find your periods:
- Last longer or may only last a couple of days
- May be heavier or lighter than normal
- Are more frequent – every 2 weeks – or less frequent
Some months you may not notice any changes, and other months you may notice that your periods are different. It is worth keeping a diary of your periods to see if they are changing as this is a clear indication that you may be entering the perimenopause.
It is estimated that up to 60% of women experience moderate to severe vaginal dryness because of menopause.
Vaginal dryness is caused by a reduction in oestradiol, a type of oestrogen, during the perimenopause and menopause. Vaginal dryness can cause an itchy or sore vagina, pain or discomfort during sex, a need to pee more often and can make you more susceptible to urinary tract infections.
Women may experience the need to go to the toilet more often, or in some cases lose control of their bladder during the perimenopause. This is because the vagina and urethra lose their elasticity and the pelvic muscles become weaker. In addition, women may experience more urinary tract infections (UTIs) due to lower levels of oestrogen.
The unpredictable spikes and falls in both oestrogen and progesterone during the perimenopause can cause breast soreness.
Breast pain as a symptom of the perimenopause feels different from the type of pain experienced just before your period. Breast pain during the perimenopause feels like a burning sensation or soreness, it can also feel like a sharp, stabbing or throbbing pain. It may be felt in both breasts or just one breast.
Once women have reached the menopause and their periods have stopped, breast pain should ease off and no longer cause any discomfort.
If you are ever concerned about changes to your breasts you should make an appointment with your GP. The NHS also offer free mammograms to women over the age of 50.
Reduced sex drive or a loss of libido is common during and after the menopause affecting 20-40% of women.
“It can be one of the most difficult symptoms to manage. This is often because the woman doesn’t understand why it’s is happening and what to do about it,” says Trudy Hannington, a psychosexual therapist at the Leger Clinic.
Vaginal dryness along with other symptoms such as sore breasts, fatigue, hot flushes can all impact a woman’s desire to have sex.
Low oestrogen levels can result in less fluctuating cortisol levels which increases blood sugars and slows down digestion. As oestrogen plays a role in the function of the gastrointestinal system, low levels can cause bloating, indigestion, acid reflux, stomach cramps along with nausea, flatulence, constipation, and diarrhoea.
Hormonal changes during the perimenopause often mean women gain weight, particularly around their abdomen. On average women gain 4-7lbs in weight during the menopause.
Due to the declining levels of oestrogen, the body tries to produce more of this hormone from elsewhere in the body. It does this via the fat cells (adipose cells), as such, the female body may need to be fatter for this to happen.
Our guide to menopause diets has more information on how you can manage your weight during menopause.
Hot flushes and night sweats are the same, the only difference is that night sweats are hot flushes that happen at night.
Hot flushes and night sweats are caused by declining oestrogen levels, this impacts your brains’ ability to regulate body temperature. Your body thinks it is overheating when it isn’t and your brain triggers the body to cool down by sweating and increasing blood flow through the skin’s blood vessels which causes the flush.
Hot flushes and night sweats are common menopausal symptoms and can vary in severity and duration. For about 20% of women, they can be quite severe and cause a lot of distress impacting work, sleep, and overall quality of life. However, for most women going through the menopause, they only occur occasionally.
Experiencing hot flushes and night sweats can also increase body odour. In addition, symptoms such as anxiety create sweat produced in the apocrine glands. Anxiety sweat is fatty and breeds and feeds on bacteria which creates a more pungent smell.
During the perimenopause, levels of the hormones oestrogen and progesterone fluctuate and gradually decline as a woman nears the menopause. These hormone changes can have a drastic impact on sleep.
“Estimates are that between 40 and 60 per cent of women will be affected by insomnia or another sleep disruption,” says Dr Heather Currie, founder of Menopause Matters.
Oestrogen is important for managing the level of magnesium in the body. Magnesium is used by the body to help muscles relax and low levels can make it more difficult to fall asleep. In addition, falling oestrogen levels cause hot flushes and night sweats which can also impact the natural sleep cycle.
Progesterone also plays a key role in as it helps you fall asleep and stay asleep. Fluctuating and declining levels of this hormone will make it more difficult to slip into a deep sleep. It can also impact the quality of sleep, making you feel tired in the morning.
Other perimenopause symptoms such as night sweats, joint aches, and the need to urinate more frequently all impact a good night’s sleep, resulting in fatigue and tiredness during the day.
Tiredness and fatigue have an impact on being able to carry out and cope with day to day tasks and life events. This can result in stress which in turn increases levels of the stress hormone cortisol in the body – raised cortisol levels, particularly at night will impact your ability to fall asleep and stay asleep.
In addition, low levels of oestrogen can also result in a feeling of fatigue.
Research indicated that 61% of perimenopausal women experienced low mood.
Sleep problems caused by perimenopause symptoms such as night sweats, lead to sleep deprivation which in turn can cause anxiety and/or depression.
“Neuroscientists have found that sleep deprivation fires up areas of the brain associated with emotional processing. The resulting pattern mimics the abnormal neural activity seen in anxiety disorders” according to PsychCentral.com.
In addition to poor sleep quality, anxiety, and depression, along with low mood are associated with low levels of serotonin. Oestrogen influences the production and breakdown of serotonin, so lower levels of oestrogen will impact serotonin levels in women going through the menopause.
Poor sleep can also have an impact on your levels of the stress hormone cortisol. Your cortisol levels rise and fall throughout the day, with levels being higher first thing in the morning. But a lack of sleep can cause your cortisol levels to rise and stay high which can impact mood, including feelings of anxiety and depression.
Memory loss or lapses, trouble concentrating and the feeling of ‘brain fog’ can be worrying but are natural symptoms of the perimenopause and menopause. Up to 47% of the women we surveyed experienced ‘brain fog’, reduced memory and concentration during the menopause.
It’s a symptom many women do not often associate with the early stages of the menopause – instead of putting it down to being too busy or stressed with work or life in general.
Our own research looking at women in the workplace has shown that 43% of menopausal women experience memory issues while at work.
Across all cultures, 34-62% of women experience menopause-related memory changes which often mimic the symptoms associated with early signs of dementia.
A drop in oestrogen levels can result in a lack of focus and concentration, but other symptoms associated with the menopause can also cause memory and concentration issues.
Sleep deprivation as a result of poor sleep caused by night sweats and other symptoms; anxiety and increased stress levels due to a lack of sleep can all impact cognitive function and could be the cause of memory issues, trouble concentrating and ‘brain fog’.
Have you ever woken up first thing in the morning to the room spinning as if you’ve had one too many the night before? This feeling is known as vertigo and, along with dizziness, is another symptom of the perimenopause caused by a drop in oestrogen levels.
Declining oestrogen levels can impact blood circulation, the nervous system and blood pressure by reducing the reactivity of the artery walls. This, in turn, affects the brain resulting in dizzy spells.
Falling oestrogen and progesterone levels are also the cause of headaches in menopausal women and some women may even experience migraines for the first time during perimenopause. Women who suffer from headaches around their period due to low oestrogen levels may find headaches increase as they transition to the menopause. But after menopause, some women find that headaches, in particular, migraines lessen.
Oestrogen and progesterone level fluctuations can be responsible for the aches and pains women feel as they transition through the menopause. There are oestrogen and progesterone receptors all over our bodies including joints, and as oestrogen and progesterone levels fall, this can cause joint inflammation.
Women may notice their hair becoming thinner or even hair loss during the perimenopause, as well as brittle nails and dry, itchy skin or acne breakouts.
This is due to the declining levels of oestrogen and progesterone which can affect hair growth, causing it to grow more slowly, become thinner and even fall out.
In addition, as oestrogen and progesterone levels fall, this triggers a group of hormones called androgens to increase. Androgens are known as male hormones and include testosterone and androstenedione and are present in both men and women. In women, an increase in these hormones can shrink hair follicles causing hair loss, but excess levels can also result in hair growth in unwanted places such as on the face.
Brittle nails are caused by weakening keratin layers. Keratin is a protein that nails are made up of but drops in oestrogen weaken the keratin layer of the nail causing it to break more easily. Dehydration can also cause nails to become dry and break more easily.
Oestrogen is associated with the production of collagen, as well as the production of natural oils that keep our skin supple and prevents it from drying out. As oestrogen levels drop, this impacts the creation of collagen and natural oils in our skin causing it to become dry and itchy.
Some women even experience acne during the menopause caused by a decrease in oestrogen and an increase in testosterone.
Is there an impact on Long-term health?
As well as the drop in oestrogen levels, menopause causes changes to the metabolism and cardiovascular system. This increases your risk of developing:
- Cardiovascular disease
- Cancer
- Metabolic diseases
- Osteoporosis
However, understanding these risks early on means you can make lifestyle changes to help improve your health in later life. Even if you are post-menopausal, there are changes you can make to your diet and lifestyle to ensure you stay fit and healthy.
“With increasing life expectancy, women are spending more time of their life in the menopausal state. So, looking for strategies to enjoy this part of your life is time well spent.”, Dr Nicky Keay, Forth Chief Medical Officer
How to cope with symptoms & improve long-term health
There are a number of ways to manage the symptoms of the perimenopause. These include:
- Ensuring you have a healthy, balanced diet with plenty of fresh fruit and vegetables, lean meat, and unsaturated fat
- Reducing your intake of caffeine, alcohol and sugary foods
- Getting regular exercise which can help with symptoms such as hot flushes and low mood. It is also important to protect bone and cardiovascular health
- Hormone replacement therapy (HRT) is used to help relieve perimenopause symptoms as well as safe guard longer term health
- Non-hormonal remedies such as Black Cohosh, St John’s Wort and Rhodiola Rosea can also help with some of the symptoms such as hot flushes and low mood
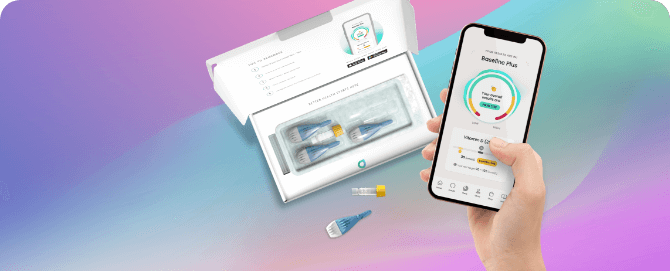
MyFORM® Perimenopause Test
Our ground-breaking perimenopause blood test maps your hormones across your entire menstrual cycle, helping you to confirm whether you’re in perimenopause, and the strength of your ovarian response.
Breakthrough Test
MyFORM® Perimenopause Test

Understand if symptoms you're experiencing could be due to perimenopause with our ground-breaking hormone mapping test.
Female hormone mapping
Tracked 24 delivery & return
Two test kit
£129
3 interest-free payments of £43
- Health scores calculated
Close
This article was written by Forth
This information has been medically reviewed by Dr Thom Phillips
Thom works in NHS general practice and has a decade of experience working in both male and female elite sport. He has a background in exercise physiology and has published research into fatigue biomarkers.

Dr Thom Phillips
Head of Clinical Services
Get 10% off your first test
Sign up to offers and all the latest information on managing your own health and save 10% on your first test.