9 mins read
Menstrual Cycle: Tune Into Your Hormones

Every woman can expect to experience up to 480 monthly fluctuations in their female hormones over a menstrual cycle.
So, how can women gain insights on the impact these fluctuating hormones have on their health and wellbeing over their life, or if their hormones are fluctuating as they should?
In this article we take a look at the impact hormone variations during the menstrual cycle can have on women’s wellbeing. We also provide a solution for women wanting to tune into their hormones. Whether it’s to improve and optimise overall wellbeing and exercise performance, navigate perimenopause or help manage conditions dependent on female hormones such as fertility issues, PCOS, or PMS – our new advanced female hormone blood test, MyFORM™, can help. Keep on reading to find out more.
View our Hormone Tests and start your journey to better health today
The Menstrual Cycle
Most women will experience menstrual cycles for at least 30 years of their lives. During each menstrual cycle, female hormone levels rise and fall significantly in an intricate web of internal feedback mechanisms that regulate the release of an egg from the ovaries.
Menstruation (periods) heralds the start of each menstrual cycle and occur in women from the early teenage years through to the menopause, when menstrual periods stop. The average age of the first menstrual period (otherwise known as menarche) is around 12 years old. Menarche can occur a few years before or after the average age, but not later than 16 years of age.
Outside of pregnancy, women will continue to have regular periods during their adult lives until they enter the early stages of the menopause known as perimenopause. During perimenopause, normal hormone fluctuations begin to change as the ovaries become less responsive.
Perimenopause ends with menopause which is when a woman hasn’t had a period in over 12 months. The average age of menopause is 51, however, there can be variations of a few years either side of this, though menopause does not usually happen before the age of forty-five.
How Long Is The Menstrual Cycle?
On average a menstrual cycle lasts 28 days, but the range in length tends to be around 24 to 35 days, with women having at least 9 menstrual periods per calendar year.
What Are The Menstrual Cycle Phases?
The menstrual cycle is the regular cycle of changing hormones in women and is made up of 2 phases, the follicular phase and luteal phase.
The start of a menstrual cycle, day 1, is the first day of the menstrual period bleed. From this day 1 up to ovulation (which occurs roughly mid cycle day 14) is referred to as the follicular phase.
During this first phase of the menstrual cycle, a follicle in the ovary starts developing to release an egg from the ovary at ovulation. This produces oestrogen (the most active form of which is oestradiol), which is the dominant hormone during the follicular phase of the menstrual cycle.
The time from ovulation to the start of the next menstrual period is the luteal phase. During this second phase of the menstrual cycle the remnants of the follicle from which the egg was released forms the corpus luteum in the ovary. The corpus luteum produces progesterone which is the dominant hormone during the luteal phase of the menstrual cycle.
Menstrual Cycle Hormones
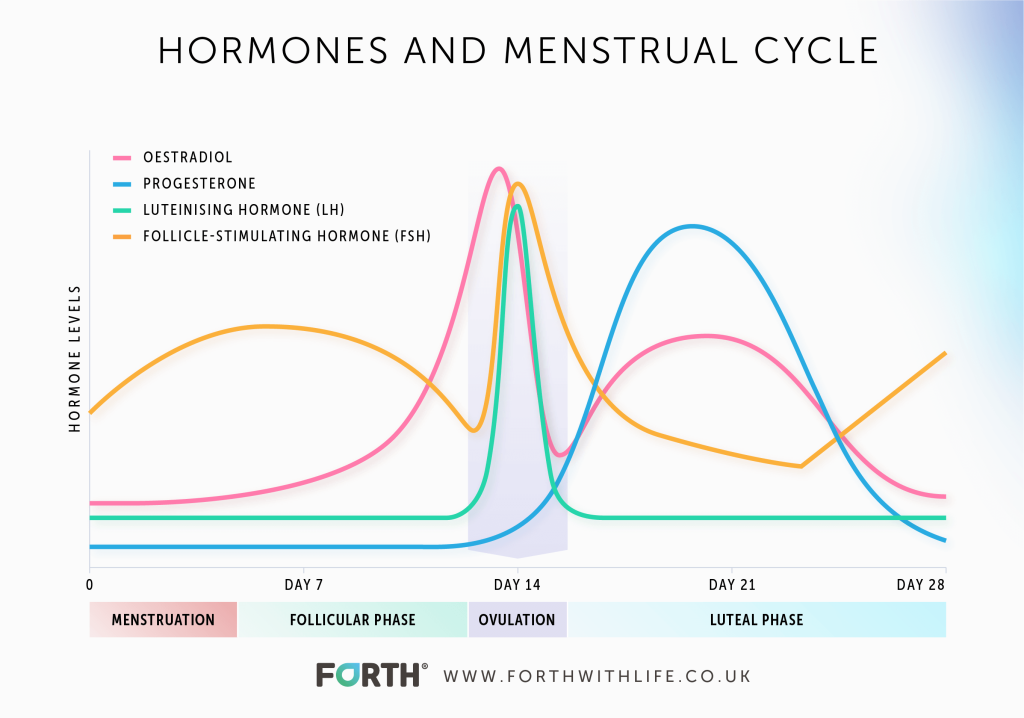
The main four hormones involved in the menstrual cycle are the two control hormones, follicle stimulating hormone (FSH) and luteinising hormone (LH), along with the ovarian response hormones, oestrogen and progesterone.
The brain is the control centre for the timing of menstrual cycles and involves the hypothalamus and pituitary glands. These release the control hormones FSH and LH in a carefully timed manner over the menstrual cycle.
These control hormones act on the ovary to produce the release of the key ovarian response hormones oestrogen and progesterone.
Check your hormones with our MyFORM™ home blood test
Hormone Fluctuations During The Menstrual Cycle
Whilst all hormones are in a dynamic state, the fluctuations of the female hormones over a menstrual cycle are the most complex and intricate of all the hormone networks.
During each menstrual cycle, female hormones vary in a characteristic pattern, shown in the menstrual cycle graph below.
How Do Female Hormones Affect Women’s Health?
Each woman’s personal and individual hormone fluctuations during a menstrual cycle shape her own unique experience in terms of physical and mental wellbeing. For example, changes in mood, sleep patterns, increased fatigue, hunger urges, or other symptoms associated with the menstrual cycle.
This is because there are receptors in the brain and other parts of the body that are affected by these hormonal variations, resulting in a range of physical and mental changes that can affect a woman’s quality of life.
This is especially true of the response hormones, oestrogen, and progesterone, produced by the ovaries. These hormones have far reaching effects on the female reproductive system, the nervous system, the musculoskeletal system, the digestive system, the cardiovascular system, the immune system, and metabolism.
Each phase of the menstrual cycle has a dominant hormone which will have an effect on a woman’s physical and mental wellbeing. For example, oestrogen is the dominant ovarian response hormone during the follicular phase of the menstrual cycle, whereas progesterone is the dominant ovarian response hormone during the luteal phase. The higher levels of progesterone during this phase causes an increase in metabolism, so it is not unusual to experience an increase in hunger urges.
In such a complex system, the length of cycles, the timing of ovulation and the precise levels of each hormone all vary from one woman to another. And to make things more complicated, an individual woman can expect to experience changes in all these variables, from one cycle to the next.
Hormone Mapping: Unique Personalisation
The current practice of measuring female hormones is to take a single blood sample, usually on day three of the menstrual cycle when hormones are at their least active. This approach gives only a single day snapshot into a woman’s hormones which, given the high level of variability over a cycle, can make it very difficult to draw any firm conclusions.
Given that hormones have such a huge impact on women’s lives, we felt more needed to be done. Working off general population averages and a single snapshot in time does not give women meaningful insights into their menstrual cycle and hormone health. This leaves women struggling for answers.
What is far more informative is knowing your own unique hormone variation over a complete menstrual cycle. By relating this information to how you feel during that cycle will provide powerful insights, giving women the answers they need.
This is exactly what MyFORM™ does, using a combination of blood analysis, artificial intelligence, and clinical expertise we have created a ground-breaking product for women.
We can mathematically model your own, personal hormone profile for each of the four key female hormones for each day of your menstrual cycle based on just 2 finger prick blood tests taken on day 14 and day 21 of your menstrual cycle.
Through machine learning, your personalised curve will adjust according to your data – the more data you input the more accurate it becomes. This will give you a tool to track your hormones throughout your different life stages. Just as if we’d taken a blood test every single day of your cycle.
Improving Female Health
Based on the connections our endocrinologist makes between your own hormone variations during your menstrual cycle and symptoms you log at the time, we provide a personalised and tailored report providing practical, real world advice on how to improve your overall health and wellbeing related to your hormones.
This advice is evidence based, focusing on factors under your control – such as nutrition and exercise – put in the context of your lifestyle and objectives.
We will also provide you with a score for overall ovarian responsiveness. We have called this the ‘Forth Ovarian Responsive Metric’ (FORM) score which calculates the balance of control (FSH and LH) and response (oestrogen and progesterone) hormones taken at the two key time points in your menstrual cycle.
Helping To Manage Conditions
Conditions such as irregular periods, premenstrual syndrome, fertility challenges, PCOS and endometriosis are associated with female hormones. MyFORM™ can help identify insufficient luteal phases and anovulatory cycles.
Helping To Identify and Navigate Perimenopause
The perimenopause is the term used to describe the transition phase to menopause when the ovaries become less responsive. This produces decreasing levels of oestrogen and progesterone and increasing levels of the control hormones FSH and LH.
These changes cause many of the symptoms women experience such as irregular periods, hot flushes, night sweats and mood changes.
By comparing your FORM score over successive cycles will indicate any change in your ovarian responsiveness. This is particularly relevant for women who may wonder if they are entering perimenopause. As perimenopause is a dynamic situation, tracking your FORM score at quarterly intervals, allows you to monitor any reduction in ovarian responsiveness, consistent with the approach of menopause.
Learn more about the menopause.
Summary
Female hormones play a huge role in women’s health. Whilst a blood test is the gold standard for measuring all 4 key female hormones, taken at a single point in time, particularly on day 3 of the menstrual cycle when these hormones are at their least active, does not provide enough information or insights into a woman’s hormone health.
Each woman’s menstrual cycle, along with the hormone fluctuations and how she feels, are unique to her. This is why a single blood test for a particular day in the menstrual cycle does not give a true picture of what is going on.
The objective of our ground-breaking MyFORM™ product is to help women understand the connection between their personal internal hormone variations and the impact this may have on their health and the way they feel. It indicates if your hormones are fluctuating throughout the month as expected and if any problems you are experiencing could be related to variations in your hormone levels.
MyFORM™ aims to help all women feel at their personal best throughout their menstrual life. For those women facing the uncertainty that occurs around perimenopause, MyFORM™ offers a greater understanding of the important changes that occur at this stage in life.
The FORM score is an important tool that can be used by women to track ovarian responsiveness over time. For women who have female hormone-related issues, such as fertility concerns and/or PCOS, MyFORM™ can also be useful.
We hope that gaining a deeper understanding of the variations in personal hormone levels over the menstrual cycle and at different stages in life will empower women to plan ahead and design strategies to achieve their own personal objectives, wherever they are in their cycle and at any stage in their life.
Read Next: ‘The Role Of Hormones In Women’s Health’
- Health scores calculated
Close
Article references
-
Bruinvels G, Burden R, Brown N, et al The prevalence and impact of heavy menstrual bleeding (menorrhagia) in elite and non-elite athletes PLoS ONE 2016;11:e0149881
-
Bruinvels G, Burden RJ, McGregor AJ et al Sport, exercise and the menstrual cycle: where is the research? British Journal of Sports Medicine 2017;51:487-488
-
Costello JT, Bieuzen F, Bleakley CM Where are all the female participants in Sports and Exercise Medicine research? Eur J Sport Sci 2014;14:847–51
-
Sheel AW Sex differences in the physiology of exercise: an integrative perspective. Exp Physiol 2016;101:211–2
-
Rymer J, Brian, K, Regan L. HRT and breast cancer risk. BMJ Editorial 2019. dx.doi. org/10.1136/bmj.l5928
This information has been medically reviewed by Dr Thom Phillips
Thom works in NHS general practice and has a decade of experience working in both male and female elite sport. He has a background in exercise physiology and has published research into fatigue biomarkers.

Dr Thom Phillips
Head of Clinical Services
Related articles
Like this article? Here are some more based on similar topics.