6 mins read
PMDD: The Impact Hormones Have on Women’s Health

We are all used to the monthly mood swings, irritability and anger outbursts that come in the 1 to 2 weeks prior to our period. We have learnt to deal with the changes our fluctuating hormones bring during our menstrual cycle. But for approximately 80,000 women in the UK – or around 5.5%– it is a lot worse. These women suffer from Premenstrual Dysmorphic Disorder or PMDD.
According to the International Association For Premenstrual Disorders (IAPMD), PMDD is a severe negative reaction in the brain to the natural fluctuations of oestrogen and progesterone during the menstrual cycle and is a suspected cellular disorder. This is what sets it apart from Premenstrual syndrome (PMS.)
PMDD & The Menstrual Cycle
PMDD occurs during the luteal phase of the menstrual cycle which is after ovulation and when progesterone levels have increased and oestrogen also starts to increase again after a peak and drop during ovulation.
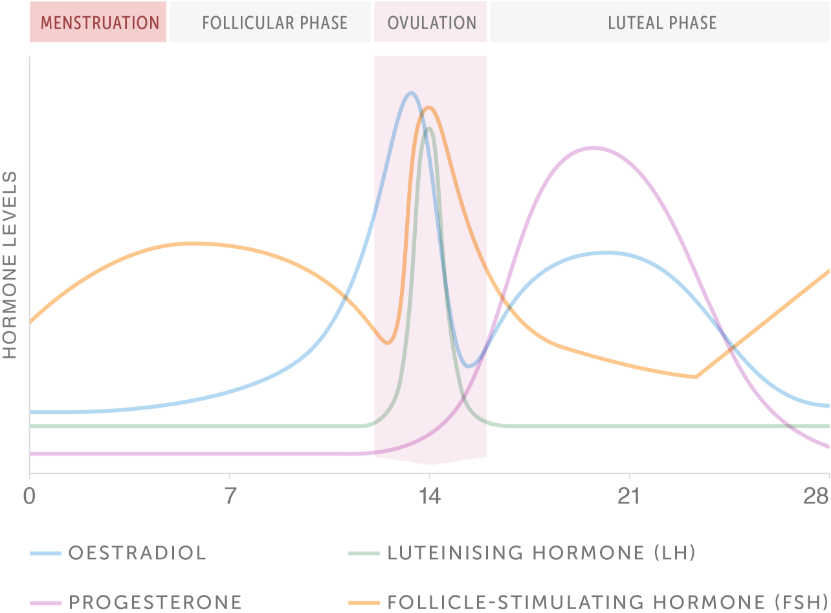
Women with PMDD experience symptoms throughout the luteal phase which can last a few days, or the 10–15-day duration prior to menstruation when symptoms subside. During this time, women’s symptoms are so severe that is impacts their quality of life – and this repeats on a monthly cycle.
What Are The Symptoms Of PMDD?
The symptoms of PMDD affect a woman emotionally as well as physically. This is because the response hormones, oestrogen, and progesterone – produced by the ovaries – have far reaching effects on all areas of a woman’s body including the nervous system, musculoskeletal system, digestive system, cardiovascular system, immune system, and metabolism, as well as the reproductive system.
The main symptoms of PMDD include:
- Mood/emotional changes (e.g., mood swings, feeling suddenly sad or tearful, or increased sensitivity to rejection)
- Irritability, anger, or increased interpersonal conflict
- Depressed mood, feelings of hopelessness, feeling worthless or guilty
- Anxiety, tension, or feelings of being on edge
- Decreased interest in regular activities (e.g., work, school, friends, hobbies)
- Difficulty concentrating, focusing, or thinking; brain fog
- Tiredness or low energy
- Changes in appetite, food cravings, overeating, or binge eating
- Hypersomnia (excessive sleepiness) or insomnia (trouble falling or staying asleep)
- Feeling overwhelmed or out of control
- Physical symptoms such as breast tenderness or swelling, joint or muscle pain, bloating or weight gain
How is PMDD Diagnosed?
According to the Royal College of Obstetricians and Gynaecologists (RCOG), PMDD is diagnosed based on symptoms. The IAPMD state that PMDD is diagnosed when a woman has at least five of the symptoms listen below with one being a ‘core emotional symptom’ (shown in bold) during their menstrual cycle:
- Mood/emotional changes (e.g., mood swings, feeling suddenly sad or tearful, or increased sensitivity to rejection)
- Irritability, anger, or increased interpersonal conflict
- Depressed mood, feelings of hopelessness, feeling worthless or guilty
- Anxiety, tension, or feelings of being keyed up or on edge
- Decreased interest in usual activities (e.g., work, school, friends, hobbies)
- Difficulty concentrating, focusing, or thinking; brain fog
- Tiredness or low energy
- Changes in appetite, food cravings, overeating, or binge eating
- Hypersomnia (excessive sleepiness) or insomnia (trouble falling or staying asleep)
- Feeling overwhelmed or out of control
- Physical symptoms such as breast tenderness or swelling, joint or muscle pain, bloating or weight gain
There are no blood tests specifically for PMDD, although RCOG recommend the use of gonadotrophin-releasing hormone (GnRH) for 3 months for a definitive diagnosis. That’s because GnRH stops the production of oestrogen.
Other blood tests, such as thyroid function, maybe carried out to rule out other disorders or hormone related conditions.
Why Are Women Struggling to Get Support For PMDD?
PMDD shares some of the same symptoms with other mental health problems such as depression and bipolar disorder. This can mean that some women are wrongly diagnosed which can lead to a longer wait time for correct diagnosis and treatment.
If you think you may be suffering from PMDD, start to keep a diary of your symptoms over the course of your menstrual cycle. Make a note of when you start your period and log your symptoms from that point through to when your period ends and you start your next period.
This will help you understand which phase of your cycle is triggering the symptoms, how long they last for and at what point during your menstrual cycle your symptoms subside. IAPMD.org have a useful symptom tracker spreadsheet you can use.
Another barrier to diagnosis and support is that many doctors haven’t heard of PMDD and are unaware of a distinction between PMS and PMDD.
Being prepared for your appointment with your GP can also help. Using an appointment sheet will help you prepare and stay focused during your visit.
If you need further support, there is help available, including:
What Is The Treatment For PMDD?
Lifestyle changes may help to control the physical and emotional symptoms, resulting in an improvement in your health. This is because the hormone network is influenced by nutrition, rest and exercise, with poor levels of either putting stress on the body which in turn impacts hormones.
Lifestyle changes may work on their own or in combination with another treatment method and are a good first step while waiting to see your GP.
Things to consider include:
- Regular exercise
- Healthy, balanced diet
- Reducing stress
- Improving sleep patterns
- Reduce your alcohol intake
- Cut down or quit smoking
- Reduce the amount of caffeine in your diet
There is no current cure for PMDD, but it is treatable through a variety of mechanisms, these include:
- Selective serotonin re-uptake inhibitors (SSRIs), a type of antidepressant
- Combined oral contraceptive pill
- Cognitive behavioral therapy (CBT)
- Painkillers/anti-inflammatories
- Gonadotropin releasing hormone (GnRH) injections
- Surgery
Some people may need to use just one or a combination of methods, but once the right balance has been found, you should notice an improvement in your symptoms.
Summary
PMDD is a severe form of PMS which has a significant impact on the quality of life of an individual living with the condition. It can cause major mood changes as well as physical symptoms, and in severe cases can lead to suicidal thoughts.
Some women find that getting a diagnosis for PMDD can take a long time due to overlapping symptoms with other mental health conditions. Some doctors are also not aware of PMDD or do not have a great understanding of the condition, which can be a barrier to diagnosis.
Thankfully, there are treatments available to help manage the symptoms and enable you to live a normal life.
Article references
-
Hantsoo, L & Epperson, C, N. (2015). Premenstrual Dysmorphic Disorder: Epidemiology and Treatment. Curr Psychiatry Rep: 17(11).
-
Freeman, E, W., DeRubeis, R, J & Rickels, K. (1996). Reliability and Validity of a Daily Diary for Premenstrual Syndrome. Psychiatry Res: 65(2).
This information has been medically written by Dr Thom Phillips
Thom works in NHS general practice and has a decade of experience working in both male and female elite sport. He has a background in exercise physiology and has published research into fatigue biomarkers.

Dr Thom Phillips
Head of Clinical Services
Related articles
Like this article? Here are some more based on similar topics.



