9 mins read
Menopause Myths – Separating Fact From Fiction

- What Is The Menopause?
- Myth Busting The Menopause
- Myth 2: It's The Menopause That Causes The Symptoms
- Myth 3: Symptoms Are The Only Way To Diagnose The Perimenopause
- Myth 4: Early 40s Is Too Young To Start The Menopause
- Myth 5: The Menopause Only Lasts A Few Years
- Myth 6: You Can't Get Pregnant
- Myth 7: HRT Has A Lot Of Health Risks
- Myth 8: You Gain
For women across the world, the menopause is an inevitable fact of life and a normal part of the ageing process. But menopause myths still exist, partly due to the menopause still being a taboo subject.
We take a look at some of these menopause myths and delve into the facts to help women have a clearer understanding of the menopause. A good place to start is with an understand of what causes the menopause.
What Is The Menopause?
As a woman gets older her ovaries become unresponsive. The two main female hormones produced by the ovaries – oestrogen and progesterone – fluctuate and gradually decline over time causing a hormone imbalance.
As the ovaries are no longer responding, the control hormones FSH and LH increase to try and get the ovaries to respond.
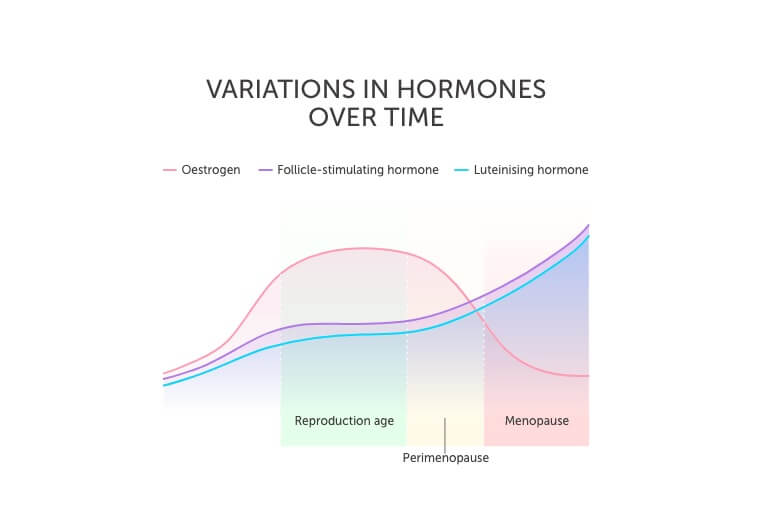
The symptoms experienced during perimenopause and menopause is the result of declining oestrogen levels.
Learn more in our Guide To The Menopause.
Myth Busting The Menopause
Here, we look at some of the common myths about the menopause and attempt to debunk them once and for all.
Myth 1: The Menopause Happens Suddenly At The Age Of 50!
This is not true. As mentioned above the menopause is due to a lack of ovarian responsiveness, which is a gradual process that lasts 4 to 8 years, starting with the perimenopause phase where most of the symptoms are experienced. Women begin to experience the perimenopause in their 40s.
Next comes the menopause, which is when a woman hasn’t had a natural period for 12 months and/or blood tests indicate lack of ovarian responsiveness.
And finally, post menopause where the symptoms can continue for an average of 4 to 5 years as hormones finally settle down – however, the symptoms are less severe.
Myth 2: It’s The Menopause That Causes The Symptoms
Even though a lot of women use the term ‘menopause’ to describe the phase in their life when they experience all the symptoms, it is the reducing responsiveness of the ovaries starting in the perimenopause phase which causes all the unpleasant symptoms.
The perimenopause is a phase that lasts several years leading up to the menopause. It’s the transition phase where FSH, LH and oestrogen levels begin to fluctuate and it’s these hormone fluctuations and gradual decline in oestrogen levels that cause the symptoms.
The term ‘menopause’ is the term used to describe the point in time when a woman’s periods have stopped for 12 months and/or blood test confirms ovaries are no longer responsive.
Myth 3: Symptoms Are The Only Way To Diagnose The Perimenopause
The symptoms of the perimenopause, such as irregular periods, hot flushes and mood swings are indicative of a woman experiencing lack of ovarian response and starting the menopause.
However, there could be other causes of these symptoms such, as an underactive thyroid. Therefore, a blood test alongside symptoms will help rule out other causes and confirm if the symptoms are related to a lack of ovarian response.
It is possible to get confirmation that your symptoms are related to hormone changes with a blood test that measures the key hormones involved in the menopause – oestrogen, FSH and LH. These hormones fluctuate during the perimenopause and cause the varied symptoms women experience. Therefore, a blood test would need to be taken over time to establish changes in hormone levels.
Read our Guide To Menopause Symptoms.
Myth 4: Early 40s Is Too Young To Start The Menopause
Unfortunately, this is not true. Women may begin to experience symptoms of the perimenopause in their early 40s. This is when hormones will begin to fluctuate and cause a variety of symptoms.
The misunderstanding and misuse of the term ‘menopause’ combined with the fact that menopause happens when a woman is in her 50s (on average, although it can happen between the ages of 45 and 55), has lead many women to think that they are too young to be going through the perimenopause in their early 40s.
This causes additional confusion when they begin to experience some of the less obvious symptoms such as anxiety, disturbed sleep and brain fog. In addition, if a woman is not keeping track of her periods, or has a Mirena coil in situ, she may not realise that they have become irregular.
In addition, around 1 in 100 women will experience the menopause before the age of 40, known as premature menopause. Premature or early menopause (before the age of 45) can occur spontaneously because the ovaries stop working or it can be induced because of chemotherapy or surgery.
It is important for women of all ages to know the signs and symptoms of the menopause and premature ovarian failure (POF). POF can occur at any age and in younger women, it can lead to serious conditions such as osteoporosis.
Myth 5: The Menopause Only Lasts A Few Years
This may be the case for some women, but in others, the symptoms may last for up to 10 years. Often, it’s easy to get bogged down in the law of averages, but each female is individual and one person’s experience may be completely different to someone else’s.
“Menopause symptoms last, on average, for between 4 – 8 years, but for a small percentage of women they may continue for longer”, explains Diane Danzebrink, The Menopause Counsellor, a psychotherapist and menopause expert. “Approximately 25% of women will experience very few or no symptoms”. Women are officially postmenopausal when 12 months have passed and no period has occurred. In fact, most women spend one-third of their life postmenopausal.
Myth 6: You Can’t Get Pregnant
This is not true, while a woman is still having periods, regardless of how irregular they are, she should continue to take some form of contraception.
A woman should continue with her usual contraception routine until she hasn’t had a natural period for 12 months if over the age of 50. By this time, a woman is considered to have reached the menopause. If a woman reaches menopause before the age of 50, then she should continue to use contraception for two years without a natural period.
Women should consult their GP to get more advice on contraception as they transition through the menopause.
Myth 7: HRT Has A Lot Of Health Risks
The HRT debate is massive and the adverse health claims are constant, but let’s first take a look at what HRT is.
HRT stands for hormone replacement therapy and is a treatment prescribed to women going through the menopause to help alleviate some of the symptoms. There are two types of HRT:
- Combined HRT which includes oestrogen and progesterone
- Oestrogen-only HRT which is only suitable for women who have had a hysterectomy
Oestrogen on its own can increase the risk of womb cancer, which is why progesterone is always prescribed alongside oestrogen unless a woman has had a hysterectomy.
HRT can also help protect against long term health issues such as osteoporosis. The decrease of oestrogen in the body leads to a loss of bone density. This is why it’s important for women to eat a healthy, balanced diet, take vitamin D and ensure they continue to exercise – especially weight-bearing exercises.
HRT, therefore, is the most widely used treatment to combat the symptoms of the menopause. Yet, there have been concerns raised about HRT including the fact it may increase the risk of breast cancer, ovarian cancer and heart disease.
“The disadvantages of HRT have been focused on the much-reported increased risk of breast cancer, however, it is important to put this into context. The increased risk is only related to some forms of HRT and Cancer Research UK state that the risk is small compared to many lifestyle risk factors including smoking, being overweight or drinking alcohol”, says Diane Danzebrink, founder of Menopause Support UK and media spokesperson for the Royal College of Obstetricians and Gynaecologists
In 2016 NICE changed its guidelines1 to encourage doctors to prescribe HRT to their patients and relieve their symptoms. NICE states women should be told2:
- The risk of venous thromboembolism is greater for oral HRT than transdermal HRT (skin patches)
- HRT doesn’t increase the risk of heart disease when it is begun in women under the age of 60
- HRT doesn’t affect the risk of dying from cardiovascular disease
- Oestrogen-only HRT is associated with little or no change in the risk of breast cancer
- HRT that contains oestrogen and progestogen may increase breast cancer risk. This risk may be higher if you take HRT for longer but falls again when you stop taking HRT.
Diane continues, “the benefits of taking HRT are that it can help to improve menopause symptoms and offer protection for long term health. Many women are reluctant to try HRT due to the myths that have grown up out of the negative press, but once they start to use it and find the right preparation and dose for them many report being back to themselves and having their lives back.”
Read our guide to Hormone Replacement Therapy.
Myth 8: You Gain Excessive Weight During The Menopause
This is not true. It is common for some women to gain around 4-7lbs in weight, especially in underweight women. However, the menopause does not cause excessive weight gain.
Women may find that they have more weight around their stomach which is caused by hormonal changes that result in a redistribution of fat within the body.
Learn more about menopause and weight gain.
Summary
The menopause can be a very confusing time in a woman’s life, made worse by the lack of education women receive around the menopause and what to expect.
“When it comes to managing your menopause symptoms it is important to have factual, evidence-based advice upon which to make an informed decision. In November 2015, NICE produced menopause guidelines for clinicians but they are available for everyone to read. I would highly recommend having a look at them before you seek advice from your GP so that you know what information and choices should be on offer to you”, says Diane.
Thanks to an increased awareness of the menopause, and it being spoken about more openly by people like Louise Minchin from BBC Breakfast, more is being done to break down the barriers and prevent the menopause being a taboo subject.
It is important that women educate themselves on the menopause and what to expect. Women should try and talk to their mother, grandmother and friends to learn more about this natural part of life.
We have created a comprehensive guide to the menopause to help women of all ages understand this part of their life.
Article references
-
Faubion, S, S et al. (2017). Genitourinary Syndrome of Menopause: Management Strategies for the Clinician. Mayo Clin Proc: 92(12), pp 1842-1849.
-
Newson, L. (2016). Myths and Misconceptions of the Menopause. British Journal of Family Medicine: 4(6).
-
Shuster, L, T et al. (2010). Premature Menopause or Early Menopause: Long-Term Health Consequences. Maturitas: 65(2).
This information has been medically reviewed by Dr Thom Phillips
Thom works in NHS general practice and has a decade of experience working in both male and female elite sport. He has a background in exercise physiology and has published research into fatigue biomarkers.

Dr Thom Phillips
Head of Clinical Services
Related articles
Like this article? Here are some more based on similar topics.


