10 mins read
What Hormones Are Included In A Female Hormone Test?
- What Hormones Can Be Measured In A Female Hormone Test?
- What Do Female Hormone Test Results Tell You?
- What FSH And LH Test Results Mean
There are different kinds of female hormone tests that cover fertility, hormone imbalance, perimenopause, and menopause.
Our guide to female hormones takes a look at some of the common hormone biomarkers used in female hormone tests and what they tell you about your hormone health.
What Hormones Can Be Measured In A Female Hormone Test?
The hormones measured in female hormone tests can include:
- Follicular Stimulating Hormone (FSH)
- Luteinising Hormone (LH)
- Oestrogen (Oestradiol)
- Progesterone
- Testosterone
- Sex Hormone Binding Globulin (SHBG)
- Thyroid Hormones (TSH, T4, T3)
Let’s take a look at each of these hormones and what insights they provide on a woman’s health and wellbeing.
What Do Female Hormone Test Results Tell You?
It is worth ensuring that any test you use is measuring all 4 key hormones which are responsible for ovarian response – these include the two control hormones FSH and LH as well as the 2 ovarian response hormones oestrogen and progesterone.
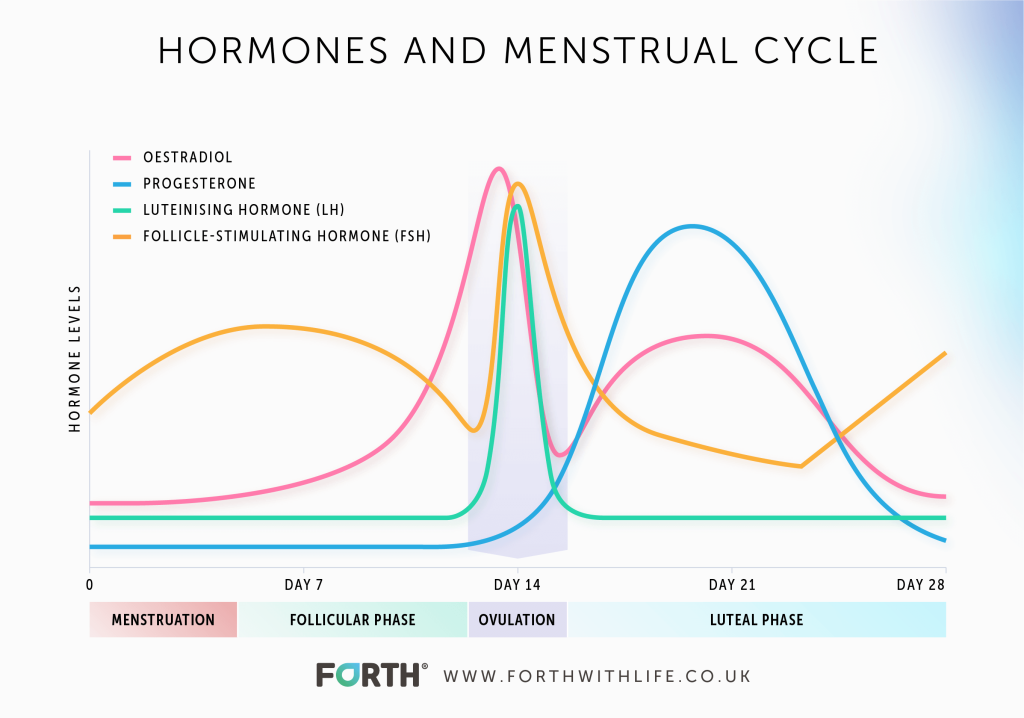
This network of hormones move in a complex but characteristic pattern across the menstrual cycle, so measuring all 4 hormones is key in gaining a clear understanding of your hormone health which influences so many other aspects of your wellbeing beyond fertility.
The graph below shows how these 4 hormones normally fluctuate throughout a menstrual scale. The exact timings will fluctuate accordingly to an individual woman’s cycle length.
1. Follicular Stimulating Hormone (FSH) & Luteinising Hormone (LH)
What FSH And LH Do
Follicle stimulating hormone (FSH) and luteinising hormone (LH) are the two control hormones produced in the pituitary gland in the brain.
FSH and LH work together to stimulate the growth of ovarian follicles and the release of an egg. FSH stimulates the ovarian follicle causing an egg to grow – this is the follicular phase which is the first phase of the menstrual cycle – and triggers the production of oestrogen in the follicle.
The rise in oestrogen during the follicular phase triggers the pituitary gland to stop producing FSH and to start producing LH. The surge in LH causes the ovaries to release the egg, a process called ovulation. This is why tests like our advanced female hormone blood test, MyFORM™, measure the LH surge as an indicator of ovulation occurring around day 14 of your cycle.
After ovulation, the remaining ovarian follicle forms a corpus luteum and LH stimulates the corpus luteum to produce progesterone in the second phase of your cycle called the luteal phase.
What FSH And LH Test Results Mean
High levels of LH and FSH can indicate a lack of ovarian responsiveness and can be a sign of ovarian failure. Increased FSH and LH levels associated with high LH levels can indicate Polycystic Ovary Syndrome or in women over 40 can indicate transition towards the menopause, known as the perimenopause, when ovarian responsiveness will start to decline.
2. Oestrogen
What Oestrogen Does
Oestrogen is triggered by FSH during the follicular phase of a woman’s menstrual cycle. Oestrogen enables an egg to mature and to be released from the ovary.
Oestrogen is also responsible for the thickening of the uterus lining to enable the fertilised egg to implant itself and develop into a foetus. If fertilisation doesn’t take place, then oestrogen levels decline prior to menstruation.
What Oestrogen Test Results Mean
Oestradiol (E2) is the main form of oestrogen in a woman’s body and plays a role in all aspects of her health, not just reproduction.
There are oestrogen receptors throughout the body and oestrogen plays a role in the regulation of physiological and psychological functions such as bone density, brain function, cardiovascular system, central nervous system, and immune system.
Women going through the perimenopause will start to experience declining levels of oestrogen due to the ovaries becoming less responsive as a woman gets older. This is the main cause of perimenopause symptoms such as irregular periods, hot flushes, mood changes etc.
Low oestrogen levels in women under 40 can be caused by excessive exercise, eating disorders, low-functioning pituitary gland and premature ovarian failure.
Abnormally high oestrogen levels in relation to progesterone is a condition known as oestrogen dominance and can be caused by medication such as hormone replacement therapy or the oral contraceptive pill.
Learn more ‘Why Oestrogen Is The True Power Hormone’.
3. Progesterone
What Progesterone Does
LH stimulates the corpus luteum to produce progesterone after ovulation. Progesterone is needed to sustain the early stages of pregnancy if an egg is fertilised. Progesterone thickens the lining of the womb in preparation for the fertilised egg to implant into the womb lining.
If the egg has been fertilised, then the corpus luteum continues to produce progesterone until a few weeks into the pregnancy when the placenta starts to be the main source of progesterone. The placenta produces high amounts of progesterone to help maintain the pregnancy.
If the egg isn’t fertilised, levels of FSH and LH fall, and menstruation occurs.
You can see how all 4 of these hormones – FSH, LH, oestrogen, progesterone – are intricately linked, which is why it’s so important to measure all 4 in a female hormone test.

What Progesterone Test Results Mean
Progesterone is used to identify whether ovulation has occurred along with LH surge. Low progesterone levels on or around day 21 of the menstrual cycle can indicate that ovulation has not occurred.
Low progesterone levels during pregnancy should be investigated as it could indicate that the body will struggle to maintain the pregnancy full term. Symptoms of low progesterone during pregnancy include spotting and miscarriage, low levels can also indicate an ectopic pregnancy.
If you are not pregnant, signs of low progesterone levels include headaches or migraines, mood changes including anxiety or depression and irregular periods. If a woman is having irregular or no periods with low progesterone, then this could also indicate a lack of ovarian responsiveness.
As mentioned above, low progesterone levels can cause oestrogen dominance causing symptoms such as weight gain, low libido, mood changes, irregular periods or heavy periods and breast tenderness.
As women enter their late 30s, progesterone levels begin to decline as the ovaries become less responsive. The number and quality of follicles begin to decline causing a reduction in oestrogen levels and less ovulation [1].
This causes periods to become irregular as a woman enters her 40s with longer or shorter periods and lighter or heavier bleeds. As well as changes to her periods, declining progesterone levels, along with declining oestrogen levels cause a range of symptoms as mentioned above.
4. Testosterone
What Testosterone Does
Testosterone is a steroid hormone and is often referred to as the male hormone, but women produce testosterone too, just in smaller quantities than men. According to the British Menopause Society, young, healthy women tend to produce approximately of testosterone per day. This is 3-4x the amount of oestrogen produced by the ovaries [2].
Testosterone is produced in the ovaries and is controlled by luteinising hormone. Along with oestrogen, testosterone helps with the growth, maintenance, and repair of reproductive tissue. In addition, testosterone is used by the body to produce oestrogen.
Testosterone levels remain relatively stable throughout the menstrual cycle with a slight increase during ovulation. Levels of testosterone naturally decline as a woman gets older.
Testosterone plays a wide role in women’s health by promoting muscle and bone strength, brain function, fat distribution, heart function, blood vessels production, energy levels and sex drive.

What Testosterone Test Results Mean
Low testosterone levels can impact women in a variety of ways due to its wide role throughout the body. It not only affects fertility, but sex drive, energy levels causing tiredness or fatigue, mood changes such as anxiety or depression, headaches, weight gain, irregular periods, vaginal dryness cognitive problems, loss of bone density, and sarcopenia (generalised loss of skeletal muscle mass and strength).
Low testosterone levels in pre-menopausal women can be caused by chronic stress or thyroid issues [3].
High levels of testosterone can be caused by high insulin in the ovaries. In addition, high testosterone can also be a sign of PCOS which affects the functioning of the ovaries and results in irregular periods and trouble conceiving. PCOS is commonly linked to insulin imbalance as well, causing high testosterone levels [4].
Signs of high testosterone levels include:
- Irregular periods
- Increase in body hair, particularly on the face
- Acne
- Balding
- Low sex drive
- Mood changes – anxiety or depression
- Deeper voice
- Increased muscle mass
- Decreased breast size
High levels of testosterone should be investigated further by a healthcare professional.
5. Sex Hormone Binding Globulin (SHBG)
What SHBG Does
SHBG is a protein made by the liver and binds to oestrogen, dihydrotestosterone and testosterone to carry these hormones throughout the body.
SHBG controls the amount of testosterone that the body tissues can use so is often measured alongside testosterone. Once these hormones bind to this protein, they become inactive and are unavailable for the body to use. SHBG levels are generally higher in women than men, meaning that women have lower levels of testosterone available for their body to use.
SHBG is used to measure how much testosterone is being used by the body, this differs from a total testosterone test which measures the amount of testosterone there is in the body.
What SHBG Test Results Mean
Low levels of SHBG means that there is more testosterone available for body tissues to use and therefore leads to high testosterone levels. An SHBG is often measured alongside testosterone or an SHBG test might be carried out if you have symptoms of abnormal testosterone levels.
6. Thyroid Hormones
What Thyroid Hormones Do
Thyroid tests are generally made up of thyroid stimulating hormone (TSH), Thyroxine (T4), Triiodothyronine (T3) and thyroid antibodies – thyroglobulin, and thyroid peroxidase (TPO).
The main function of the thyroid stimulating hormone is to regulate thyroid function. T3 and T4 play a role in the body’s metabolic rate. TPO has an important role in the production of thyroid hormones. Thyroglobulin aids in the production of both T3 and T4.
What Thyroid Test Results Mean
These biomarkers are used to test for thyroid problems such as an under-active or overactive thyroid.
Increased levels of thyroid antibodies indicate that your thyroid gland is under attack from your immune system, which can impact the proper functioning of your thyroid gland. Having raised antibodies can increase your risk of going on to develop a thyroid disorder and can indicate an autoimmune condition.
High levels of thyroid stimulating hormone and thyroxine can indicate an underactive thyroid which can lead to fatigue and weight gain.
Low levels of TSH and thyroxine are often associated with an overactive thyroid which can cause mood swings and difficulty in sleeping.
The symptoms of an overactive thyroid are:
- Changes in mood
- Anxiety
- Nervousness
- Difficulty sleeping
- Irregular or fast heartbeat
- Weight loss
- Trembling
- Increased risk of cardiovascular risk
- Swelling in the neck, goitre
The symptoms of an underactive thyroid, include:
- Fatigue
- Weight gain
- Dry skin and hair
- Depression
- Muscle aches
- Sensitivity to the cold
Women are more likely to suffer from thyroid issues than men, which is why it’s often included in a female hormone test. Symptoms of a thyroid disorder can be similar to symptoms of the perimenopause. According to the NHS, 1 in 50 women have an overactive thyroid also known as hyperthyroidism and are 6x more likely to suffer from it than men.
Summary
The four main sex hormones – LH, FSH, oestrogen and progesterone – are intricately linked in a hormone network that fluctuates naturally across a menstrual cycle. These hormones also change throughout a woman’s life, from early reproductive age to menopause.
To have a good understanding of what is going on with hormone health you should use tests that measure all 4 of these hormones.
There are additional biomarkers such as testosterone, SHBG and thyroid hormones which also contribute to a woman’s overall wellbeing and are often included in tests to help identify issues related to fertility such as PCOS or thyroid disorders.
- Health scores calculated
Close
Article references
This information has been medically written by Dr Thom Phillips
Thom works in NHS general practice and has a decade of experience working in both male and female elite sport. He has a background in exercise physiology and has published research into fatigue biomarkers.

Dr Thom Phillips
Head of Clinical Services
Related articles
Like this article? Here are some more based on similar topics.